CDC’s Guidance Changes The Way Prince George’s County Approaches COVID-19.
Newsletter Sign Up
〰️
Newsletter Sign Up 〰️
On Feb. 25, the same day the CDC announced that it was changing its community transmission metrics, Prince George’s County, County Executive Angela Alsobrooks and local health officials announced that the county was rescinding its indoor mask mandate, except on public transportation. “From the very beginning of the pandemic, we said that we would listen to the experts,” said Alsobrooks. “I promised you that we would make all our decisions on science, and medicine; that we would be guided by data, and that we would follow what that data said. The latest data, which reveals our low transmission and positivity rates, ...have led us to decide that we are lifting the indoor mask mandates, effective Feb.28. I have waited a long time to say that it is safe for us to do this.”
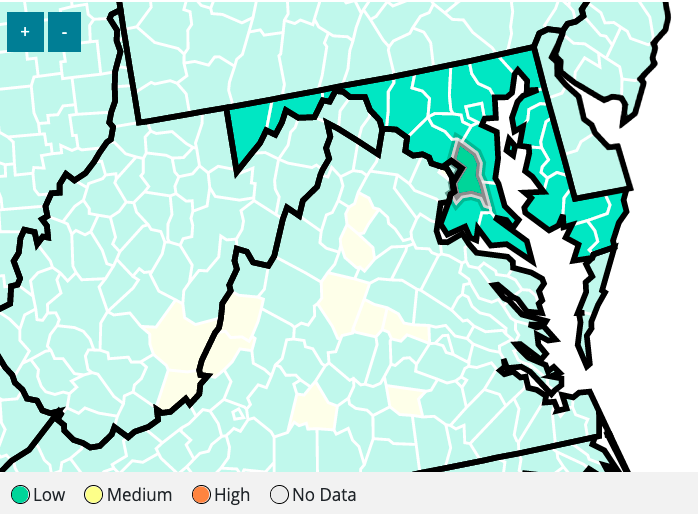
The old CDC’s community transmission metrics had a color-coded system that gave local public health officials an early warning when community spread was at a dangerous level. The CDC replaced it with a new metric system, raising the community threshold, which allows the county’s commission spread to remain low, even when other metrics say otherwise. Some public health experts have warned that rescinding the mask mandate puts those who are vulnerable to the virus at risk. They argue that CDC’s approach is not rooted in what is best for the collective, but gives individuals the freedom to choose if they want to wear a mask.
“Definitely, there is a taking away of the public from public health,” said Lakshmi Ganapathi, instructor in pediatrics at Boston Children’s Hospital. “There are individual measures and community measures that the CDC recommends. But there isn’t any concrete guidance for what entire communities need to do when there is a high community [transmission].”
Before the new changes, the CDC’s metrics included a color-coded community transmission scale based on the number of infections, per 100,000 people over seven days. A low case count was 0-10 per 100,000 people. This meant that the virus was not spreading fast, and masks were not necessary, but vaccinations were still encouraged, and social distancing was encouraged. Even though the community spread was low, the virus was still present, and people could still get infected. The goal was to keep community spread low. However, when infection cases hit 50 per 100,000 people or above, public health officials implemented indoor mask mandates, ratcheted up messaging on social distancing, and vaccinations.
The new metric erases the color-coded system. It increases the community spread threshold to 200 per 100,000 people. Up to 200 is considered low community spread. Anything beyond, 200 cases is considered high. The CDC said that it looks at the combination of three metrics: new COVID-19 admissions per 100,000 population in the past 7 days, the percent of staffed inpatient beds occupied by COVID-19 patients, and total new COVID -19 community level.
“New COVID-19 admissions and the percent of staffed inpatient beds occupied represent the current potential for strain on the health system,” CDC explains. “Data on new cases acts as an early warning indicator of potential increases in health system strain in the event of a COVID-19 surge.”
Currently, Prince George’s County, under the new metric, has a low community spread ranking. It’s for this reason that local health officials don’t seem to be alarmed about rising infection cases. However, under the old metric, the current infection rate would be considered substantial, which would require local officials to possibly reinstate a mask mandate.
Ganapathi said the new guidance puts people who have preexisting conditions, those that are immunocompromised, essential workers, the disabled, and children 0-5-years-old, who cannot be vaccinated, at risk. The metric allows for a high community spread before there is community intervention, allowing the virus to spread, and mutate. A mutated virus can evade immunity, which leads to rapid community spread. (See The Intersection’s 2021 report). The Northeast and DMV are experiencing this now with the BA.2 subvariant. A mask mandate is a community-centered prevention policy. The new metrics are individualistic, allowing people to make a personal choice about whether they want to wear a mask. For example, individuals wearing masks in rooms full of people without masks offer little protection. It still puts those vulnerable to infection in an environment where they can be infected.
“The big pitfall with the CDC guidelines is in such an event, with those thresholds, you would not prevent hospitalizations, because [public health officials] are not acting on the earlier indicators (rising COVID-19 cases),” explained Ganapathi, who has clinical expertise in immunocompromised hosts in infectious diseases. “Because you see a new variant and start to see the cases climb, by the time you get hospitalizations,...a portion of those people are going to die. This is why hospitalizations predict death. If you land in the hospital, the likelihood of you dying is higher because you were sick enough to get there.”
Public officials have argued that a new approach was needed because we have the tools - vaccines, masks, monoclonal antibodies - that mitigate infection and natural immunity to the virus. Since thousands upon thousands of Americans have been infected with the virus, people now have natural and vaccine infection immunity. Natural immunity (infection-generated immunity) is when someone has been infected with COVID-19 and their body has developed the antibodies to fight it. Vaccine immunity is when people get vaccinated and develop antibodies through the vaccine. But infection generated immunity is not a reliable way to fight the virus. You still can get the virus, which could lead to more health problems, or you could die, like so many have.
“Vaccine-generated immunity is the safer way to get immunity,” said Ganapathi. “You can certainly get immunity from infection, but the infection could kill you or could land you into very, very bad trouble. “It doesn't mean you don't get immunity after you get an infection, but it is not the best way to get the immunity when there are far safer ways to achieve the same immunity. Vaccine-generated immunity is superior to infection-generated immunity because infection-generated immunity can vary between individuals. It’s not durable, and we simply don’t know how it holds up against new variants.”
The new normal of “living with Covid-19” is accompanied by the bad idea that COVID-19 is mild. Describing COVID-19 as mild communicates that being infected with the virus does not result in severe harm because it doesn’t result in hospitalization or death. But Covid-19 infection does and has caused real harm, even when people don’t end up in the hospital or dead. Various studies have shown that infection can lead to long-term effects like shortness of breath, “subtle tissue damage, and accelerated losses in brain regions,” putting you at risk for developing diabetes, and long-COVID-19.
***
Prince George’s County health department, an economically under-resourced institution, has worked hard, alongside activists and community members, to educate residents about the vaccine and to get people vaccinated. They have put up vaccine pop shops in under-resourced Black and Latino neighborhoods. Dr. Stephen B. Thomas - professor, director of the University of Maryland’s Center for Health Equity, and one of two investigators on the Communivax study, which analyzed Prince George’s health system during the pandemic - created a program, HAIR, that engaged local barbers and salons to participate in getting locals vaccinated. The program is now nationwide. Barbers and hairdressers invited community members to a Zoom call. In that Zoom call, health professionals would help community members understand how the virus works and the importance of vaccines. Health professionals would then vaccinate people in the barbershop or salon.
Newsletter Sign Up
〰️
Newsletter Sign Up 〰️
Today, Prince George’s County is 76 percent fully vaccinated, one of the highest percentages in the state. However, only 32 percent of residents have received a booster shot. However, vaccination (2 doses) percentages are stagnant. In poorer communities, which lay within interstate 495, one-shot vaccination dosages percentages range from 53 to 60 percent, while middle to high-income neighborhoods' one-dose vaccine percentages ranges from 72 to 82 percent.
Despite this effort, Prince George’s County has been disproportionately impacted by COVID-19. Prince George’s County leads the state in COVID-19 cases and is second in total deaths after Baltimore County. The death count is likely extremely low. In the county, more men have died from COVID-19 than women. According to data compiled by The Washington Post, in DC, Maryland, and Virginia, more lower-income Black people have died from COVID-19 than those of higher income. These local trends are a microcosm of what has been happening domestically. During the Omicron surge, more African Americans were disproportionately infected by the virus and died than their white counterparts.
Though marketed as America’s Black wealthiest county, its residents still suffer under the thumb of institutional racism, producing health and resource inequities, which has resulted in a lot of negative health outcomes. Before the pandemic infected Black and brown families, were, and are still, living in a county where it has fewer hospital beds than neighboring Washington, D.C., and Montgomery County, a mostly white county. Some Black residents have little access to health facilities. The infant mortality rate is high, cancer, diabetes, and HIV, according to a Communivax study. This is not to mention other factors communities members live with, like low levels of lead in their blood. Some residents live in neighborhoods that are food deserts, and some have limited access to healthy foods. (To combat food deserts, Alsobrooks administration, small companies have built grocery stores in low-income areas where food deserts exist. There are also now new medical facilities, The University of Maryland Capital Regions Medical Center and a new cancer research facility has been built in partnership with Maryland University.) Furthermore, Prince George’s County residents are essential workers (bus/subway drivers, restaurant workers, health care workers, grocery store workers, teachers, ride-share drivers, etc.). Essential workers labored through pandemic surges, putting themselves and their communities at risk.
Not due to Black people’s genetics, but to bad healthcare systems Black people and other people of color find themselves locked in, Thomas said, “the bottom line is Black people were living sicker and dying younger before the pandemic.”
“[My] fear and concern are that by ‘going back to normal’ we’ll be back to living sicker and dying younger,” said Thomas. “We can’t let that happen. My mission right now is to make sure that we don’t go back to a normal in which Black people die younger and live sicker.”
Thomas and Dr. Sandra Crouse Quinn, professor and chair of the department of family science at the School of Public Health at the University of Maryland, interviewed people who said they had negative experiences at local health facilities, producing distrust in healthcare. I reached out to Quinn for an interview. She did not reply to my request. Researchers suggested that Prince George’s County. According to a 2019 study by Rand on Prince George’s County health residents and its healthcare system, the leading causes of death were heart disease, cancer, and stroke. Writers of the Communivax study suggested that the county keep improving its healthcare ecosystem for the betterment of its citizens.
Some children, though they are still allowed to mask indoors, live with elderly guardians, some with pre-existing conditions. Last year, I reported how parents and guardians were afraid to send their children back to school for fear of the child catching COVID-19 and bringing them back home. Parents were concerned about overcrowding in the classrooms and hallways, which did not permit students to socially distance themselves. Phyllis Wright, who was 60 years old, is the guardian of two children. She said in an education town hall meeting in 2021 that she was afraid that her children could spread the virus to her. Wright had two other relatives that died as a result of being infected.
In a scenario, due to the CDC’s new metric, and local government officials saying that the pandemic is over, where the virus is allowed to spread without intervention, will result in long-term sickness and death. As data has shown, the vulnerable are paying the price with their lives.
***
Locally, more education is needed to explain that the virus is airborne. Thomas said COVID-19 is an airborne disease, an aerosol. He said it hangs in the air like smoke. “Have you ever walked into a room after someone’s been smoking, or you walk by someone smoking on the corner ?” he asked. “ When you're by them, you can smell the smoke, even after they’ve stopped smoking.”
That is what COVID-19 is like, but, unlike smoke, it is invisible, and it doesn’t have a smell. Because those particles are present, they get inhaled, causing sickness in the body. This is how the virus is passed from one person to another.
Wearing a KN95 mask reduces infection. Along with KN95 masks, we need to equip public and private spaces with air purifiers (ventilation) to reduce the amount of COVID-19 particles in the air. He advocates for getting purifiers in public spaces: schools, barbershops, and salons. He also wants them in people’s homes. The high-end filters are expensive, and those living pay-check-to-paycheck may not afford them. He recommends that families who have the money buy parts to build to assemble the Corsi Rosenthal air purifier. However, this solution doesn’t deal with people who live in extreme poverty, and who sometimes reside in public housing. Perhaps the state can provide economic assistance to those who want to purchase the equipment.
This is not only about individual acts, but also about the CDC’s approach to public health policy. Ganapathi said public health experts who work at the federal should apply the precautionary principle. It would help local health officials to focus on early indicators (case counts and wastewater analysis). In short, the precautionary principle allows public health officials to put in measures to stave off worse outcomes, whether than waiting or acting as if the threat is not that bad. Yet, observing early indicators doesn't tell you how long a surge may or may not last. But she said there is no need to wait. If early indicators, like seeing infection cases increase through wastewater samples, for example, like in neighboring Washington, DC, then public health officials should reinstitute mask mandates, and increase testing in multiple settings, including schools.
“When you act on the early indicators, you never see the deaths that didn’t happen,” she said. “You never see the hospitalizations that didn’t happen. Early measures prevent all the things that you did not see.
Newsletter Sign Up
〰️
Newsletter Sign Up 〰️